Seeing Skincare Differently
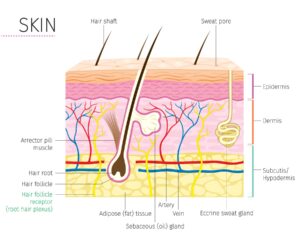
Our skin, the largest organ of our body, is much more than what we see on the surface. It’s a complex and crucial barrier that
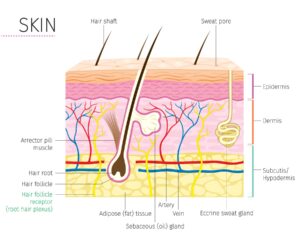
Our skin, the largest organ of our body, is much more than what we see on the surface. It’s a complex and crucial barrier that

In the world of skincare, countless products vie for our attention, promising a youthful glow, wrinkle reduction, and age defying perfection. But with so many

In the realm of skincare shopping, there’s a little-known secret that can make a big difference both to your wallet and the planet: opting for

At Columbia SkinCare, when we ponder the question, “Are you feeling well?”, we delve deep into the essence of what wellness truly signifies. In our

Most people are familiar with the nighttime ritual of using a facial moisturizer, and most people have even utilized the genius of a facial mask

How Topical Probiotics Can Benefit Your Skin The skincare industry has been essentially unchanged for generations. It has addressed skincare as a cosmetic and not

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get Anew Power Serum for $26.49 (reg.

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Fruits & Passion Cucina Hand Soap: buy

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Fruits & Passion Cucina Hand Soap: buy

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Roll-on deodorant starting at $2.69 when you

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Roll-on deodorant starting at $2.69 when you

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE belif samples with any purchase

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE belif samples with any purchase

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get our best-selling Glimmersticks eye, lip, &

Which Skincare Oil is the Best? Coconut, Jojoba, Argan Compared Right now, skin care oils are all the rage. You will hear even very esteemed skin

The EU has banned more than 1,300 ingredients, while the U.S. has banned or restricted nowhere near that amount (11). The disparity between the two

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get our best-selling Glimmersticks eye, lip, &

Is there anything more disappointing than being excited about a product just to have it cause irritation or breakouts on your skin? A true tragedy

According to dermatologist Dr. Mary P. Lupo in Allure magazine, pores cannot open and close because they have no muscular attachment. So when people say

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping on your $60+ purchase

Dear Nicki, Which is better for the skin – soap or shower gels? -Bree Dear Bree, Our great-grandparents had no choice but to use

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping on your $60+ purchase

Acne is one of the most common, yet often misunderstood, skin conditions out there. Everyone will experience a breakout at some point in their life,

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon New Avon Chi Essentials Hair Care starting

Life can be stressful and we all need ways to unwind at the end of the day. Lately, mine has been Vogue’s “Beauty Secrets” series

Dear Nicki, I love the calming properties of oatmeal the Aveeno lotions and how amazingly soft it makes my skin. Are there any similar

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon New Avon Chi Essentials Hair Care starting

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping with your $40+ purchase, ends

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping with your $40+ purchase, ends

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get our best-selling Glimmersticks eye, lip, &

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping on $25 with code

Thermage works by emitting strong waves of heat into the skin. Learn about the procedure, recovery time, cost, and other factors of Thermage!

In marketing, the term “natural” is equated to being “better.” But that isn’t always the case, according to Dr. Linda M. Katz, director of the

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping on orders $20+ with code

Thanks to social media celebrities are more accessible than ever. This is both a good and bad thing depending on who you ask. When it

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get FREE shipping on orders of $20+

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon 20% off sitewide with code SITE20, valid

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon FREE bottle of Haiku Eau de Parfum

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Our best-selling Glimmersticks eye, lip, & brow

Citric acid is in just about everything from skincare products, to food, to floor cleaner. While lemons aren’t really something you want to be rubbing

AuraGlow $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Shop the Cause! Oct. 1 – 31,

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Shop the Cause!

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Shop the Cause!

In the world of 10 and 12-step routines, sometimes we have to take a step back and ask ourselves… are we overdoing it? And when

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Shop the Cause!

If you’re like many people who have been battling acne blemishes and breakouts, you’re frustrated, tired, and embattled, having spent time and effort on countless

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

The beauty industry is booming, there is no denying that. With new brands and products popping up every day it feels like we have more

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

You’ve had a rough day at work and your mind is still racing with everything you went through and have yet to face tomorrow morning.

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

There are certain places that you expect to find fungus. Damp basements, under rocks in the woods, or grilled and served up at a steakhouse

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

AHA? BHA? Chemical exfoliation? If you’re new to skincare or trying to build your routine, these terms can be a little confusing and borderline frightening.

Recently I have been watching the Vogue Beauty Secrets series and researching celebrity skincare routines. I have noticed that many celebrities have the Dr. Barbara

AuraGlow Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with code AURA5 Avon Get up to 25%

We all love laying out by the pool on a warm summer day or spending the afternoon in the park for a family BBQ. But

Tartaric acid is another one of those often-overlooked skincare ingredients that many tend to take for granted, but this small ingredient can really pack a

AuraGlow Receive 16% off with code RVT16, ends 08/23/2019 Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with code AURA10 $5 off of order $50 or more with

The order you apply your products, the combination of products you use, and the active ingredients are all things you have to pay attention to.

AuraGlow Receive 16% off with code RVT16, ends 08/23/2019 Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with

Acne comes in all different forms and can have a multitude of different causes, ranging from hormonal to bacterial to genetic. Because of this, it

When you think of algae, images of bright green, slippery goo stuck to a rock may come to mind. It’s not something you’d want to

Putting together your skincare routine is a lot more than just knowing the proper order to use your products, which is confusing in and of

AuraGlow Receive 16% off with code RVT16, ends 08/23/2019 Receive 10% off with code REWARD10, ends 10/24/2019 $10 off of order $75 or more with

If you walk into any department store, Sephora, or Ulta there is no doubt you will see beauty product for sale marketed as “no nasties,”

Nicole Kidman is known for her beautiful porcelain skin, and she credits that to a strict sunscreen regimen. “I wouldn’t have paid any attention to

We all know that getting exercise is great for your overall health, but studies are starting to demonstrate that it can also be incredibly beneficial

Did you know that only 20% of Americans wear sunscreen? This stat has been static over the past 20 years. For most people, slathering on

Recently, a new term has arisen in skincare: “Clinical-grade.” Distinct from “professional-grade” skincare that is typically only sold at licensed professionals’ offices (think Skinceuticals), clinical-grade

In a word, no, I don’t believe that oxybenzone in sunscreen is dangerous. That said, there are skincare websites (even reputable ones) who try to

The UV Index is a tool that is used to help raise public awareness of excessive exposure to UV radiation, and instruct the general popular

Moth bean. What? Yeah. You read that right. Vigna aconitifolia is also known as moth bean, and it’s being touted as a hot new all-natural

I’ve said this before but vitamin C serums have become the Little Black Dress of skincare: It seems like everyone has one, they flatter just

Sometimes it seems as though there’s a battle raging within the skincare world about best practices for your skin. Do this — don’t do this.

As we’re about to step into July, summertime has officially begun – time for vacation! Although most of the time I admittedly work a lot,

Nowadays you can’t walk into a store that sells beauty products without seeing something formulated with CBD. From mascaras to moisturizers, it’s in just about

Acne is something that most people will struggle with at some point in their life. There’s no escaping it! In fact, an estimated 80 percent

Your skin is one of your body’s first lines of defense against foreign invasion. We rely on it to keep us safe, clean, and pure.

Sometimes, no matter how many amazing products we use, we still look at our skin and aren’t happy with the results. We think, “What else

The combination of sodium benzoate and ascorbic acid has been an ongoing topic in the food, personal care, and pharmaceutical industry for years. While both

In May of this year, the Met Gala 2019 was held in The Metropolitan Museum in New York City, with the theme of “Camp.” The

It’s the question I get asked the most here at FutureDerm: What is my skincare routine? Admittedly, even though we get sent dozens of product

What is your opinion please on very low weight hyaluronic acid (hydrolyzed sodium hyaluronate — molecular weight 10kDa) contained in some hyaluronic acid products? There

I read your reviews of the MDSUN products and I am very interested in giving them a go. I am 60 years old and am

Hey there, I have been [crawling] the internet looking for advice, and I wondered if you might be persuaded to take pity on me and

I recently had the opportunity to speak with Dr. Hooman Khorasani, Chief of Dermatologic Surgery at the Icahn School of Medicine at Mount Sinai. Here

Dear Nicki, I had a doctor peel around 15 months ago and it left me with a burn and now hyperpigmented mark on my nasal

Of all the products we’ve launched through the years, my favorite are our FutureDerm Specialist Customizable Skin Care products. And now we have partnered with

Thanks for the insightful question, L. Unfortunately, I don’t like using AHAs with retinol. I stand by this one. I’ve been called out by other

Reader question: Can I use Kojic acid cream to treat my facial skin hyperpigmentation, after I stop using hydroquinone and tretinoin in combination? Will it

Facial oils have been all of the rage for the past 3-4 years or so. Given their continued popularity, they are unlikely to go anywhere,

Before I go into this, yes, I know that I sell a vitamin C serum. (And a damn good one too!) That said, this fact

Undereye bags — A.K.A. swelling and puffiness under the eyes — are a telltale sign of aging. (The converse, sunkenness under the eyes, also tends

Recently, a reader asked me to review 7-dehydrocholesterol skincare. Think of it like a natural sunscreen. Your skin naturally contains its own supply of 7-dehydrocholesterol.

The New Year The new year comes full of promise: This year, we’re going to clean out our cabinets. Eat clean. Sleep better. Exercise daily.

Recently on Instagram, we asked you to ask me your most pressing skincare (and haircare) questions. Here are some of the questions and answers! Hi!

Of all the products we’ve launched through the years, my favorite are our FutureDerm Specialist Customizable Skin Care products. And now we have another a

Vitamin C serums have become the Little Black Dress of skincare: It seems like everyone has one, they flatter just about every skin tone, and